What is FAI (and why it feels like a “pinch” in the hip)
Femoroacetabular Impingement Syndrome (FAI) is a common cause of hip and groin pain, especially in active adults and younger athletes. It often feels like a deep ache in the groin, stiffness in the hip, or a sharp “pinch” during squats, sitting, lunging, twisting, or getting out of the car.
FAI is not automatically “bad hips.” Many people have FAI-shaped hips on scans and feel completely fine. It becomes a syndrome only when that shape, your symptoms, and tissue irritation combine to limit movement and function.

The key idea: FAI is usually a load + position problem. When the hip is repeatedly pushed into positions it can’t tolerate (often deep flexion and rotation), symptoms flare.
The goal of treatment is to calm irritation, build capacity, and restore confident movement — not to “fix” your body with fear.
What is happening inside the hip?
FAI occurs when there is repeated abnormal contact between the ball (femoral head) and socket (acetabulum) during movement. Over time, this can irritate the labrum (a cartilage rim around the socket) and increase stress on the joint cartilage.
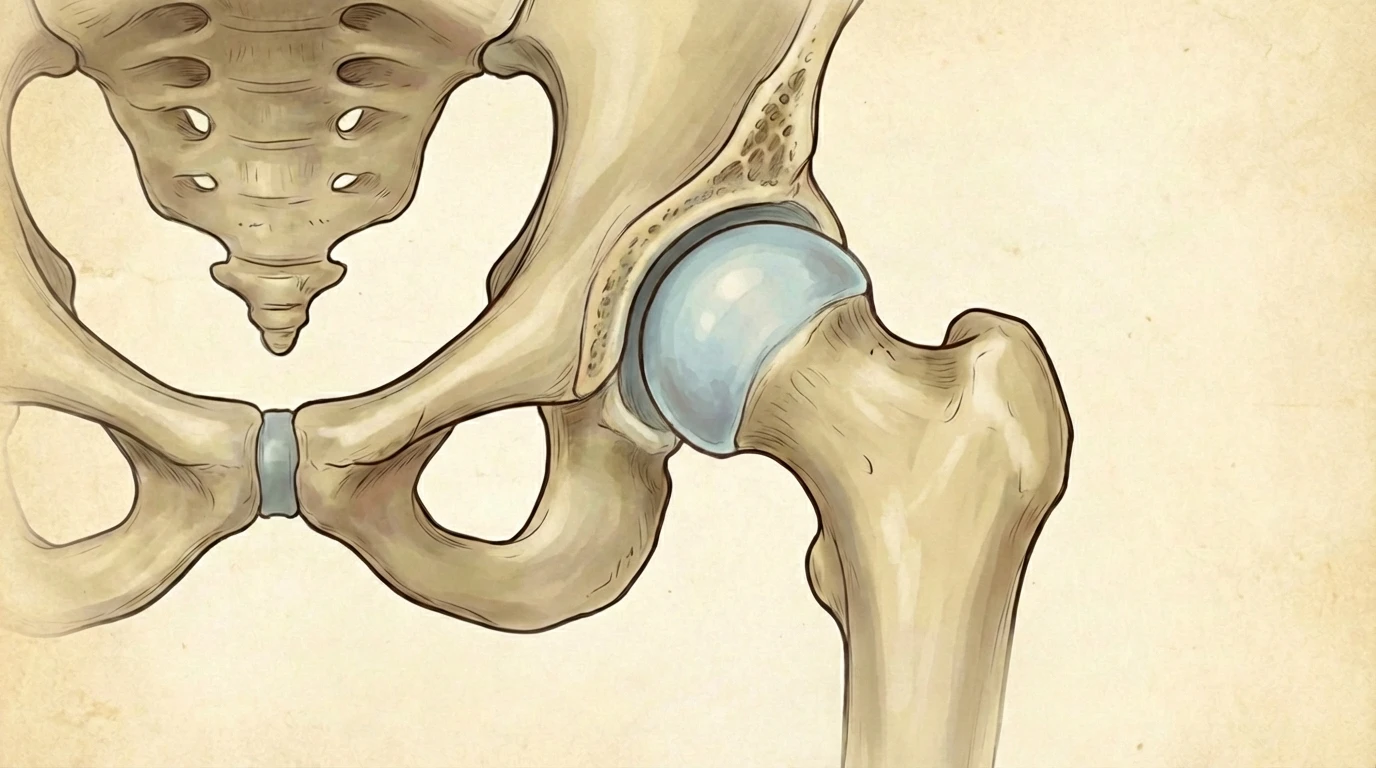
A helpful way to think about FAI: your hip may have less “clearance” in certain positions. When you repeatedly load those positions (gym, sport, sitting, work), tissues can become sensitised and irritated.
This is why two people can have the same hip shape on a scan — one has no symptoms, the other struggles. Symptoms are about tolerance and capacity, not just anatomy.
Types of FAI (cam, pincer, and mixed)
1) Cam impingement
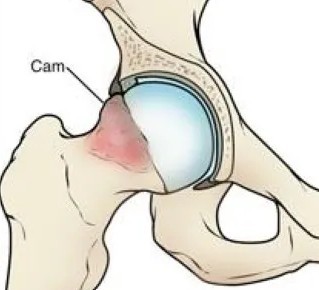
- The femoral head is not perfectly round.
- A bony “bump” can jam into the socket during hip flexion or rotation.
- Often seen in younger, active adults and athletes.
2) Pincer impingement

- The socket covers too much of the femoral head.
- This can compress the labrum during deeper hip positions.
- Often seen in adults and can occur alongside cam features.
3) Mixed FAI
Mixed FAI is the most common clinical presentation, where both cam and pincer features contribute to symptoms and movement restriction.
Common symptoms of FAI

- Deep groin pain (most common)
- Hip pain during or after activity
- Pain with sitting, squatting, lunging, or getting out of the car
- Clicking, catching, or a consistent “pinching” sensation in the front of the hip
- Reduced hip range of motion (often flexion and internal rotation)
- Symptoms with sport involving twisting, sprinting, kicking, or change of direction
What causes symptoms (and why they can appear “out of nowhere”)
FAI is usually multifactorial. Bone shape often develops during adolescence, but symptoms typically show up when the hip is repeatedly loaded in positions it can’t currently tolerate.
Key contributors can include:
- Structural factors: cam/pincer morphology developed during growth
- Movement factors: hip and pelvis control, trunk stability, technique
- Load factors: training spikes, repetitive deep hip flexion, prolonged sitting
- Capacity mismatch: doing “too much too soon” for the hip’s tolerance
How is FAI diagnosed?
Diagnosis is based on symptoms and a clinical assessment. Imaging can support the diagnosis, but it does not confirm it on its own.
1) Clinical assessment (essential)
- Hip range of motion and symptom reproduction
- Strength and control of glutes, hip rotators, and trunk
- Movement patterns (squat, lunge, stairs, running, sport-specific tasks)
- Load tolerance and training history
2) Imaging (supportive)

- X-ray: evaluates bone shape (cam/pincer features)
- MRI / MRA: assesses labrum and cartilage health
A key point: many pain-free people have FAI-shaped hips on scans. Your symptoms, exam findings, and function matter most.
Modern treatment options for FAI (best practice)
Physiotherapy is the recommended first step for most people
For many people, a structured physiotherapy program reduces symptoms and restores function. The goal is to calm irritation, improve hip mechanics, build strength and control, and progressively return you to the activities you care about.
Importantly, rehab is not “just exercises.” It is a plan that matches the right movement, load, and progression to your hip’s current tolerance.

